When I reflect on my nursing career, I vividly recall introducing evidence-based practice (EBP) in the 1990s and observing its evolution into today’s rapidly evolving healthcare landscape.
Nurses make increasingly complex clinical decisions that impact patient outcomes and safety. EBP has emerged as the gold standard approach for delivering high-quality nursing care that’s not only compassionate but also grounded in the latest research and clinical evidence.
What is evidence-based practice in nursing, and why is it essential to modern healthcare?
What Is Evidence-Based Practice in Nursing?
EBP is a problem-solving approach that integrates the latest research findings with clinical expertise to guide care and improve patient outcomes. This approach ensures nursing care quality that is current with industry standards and based on evidence rather than outdated methods. Simply put, EBP practice improves outcomes in measurable, meaningful ways.
Why Evidence-Based Practice in Nursing Is Important
Evidence-based nursing is critical to making informed decisions and delivering patient-centered care. Following best practices in nursing not only supports patients but also healthcare professionals and providers who rely on nurses to execute treatment plans. Here are some examples of EBP’s impact:
- Stronger patient outcomes: Helping nurses identify which treatments work best for specific conditions
- Decreased errors: Informing tighter nursing guidelines that decrease medication errors, hospital-acquired infections and other avoidable complications
- Standardized protocols: Offering the same high-quality care regardless of which nurse provides it
- Cost effectiveness: Eliminating ineffective treatments and streamlining care delivery to reduce unnecessary costs while maintaining quality
- Nursing research alignment: Prioritizing modern research and best practices rather than relying on outdated information
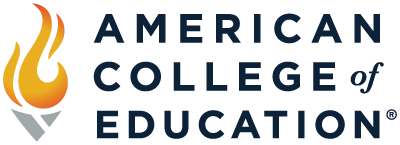
Core Components of Evidence-Based Practice in Nursing
EBP rests on three core pillars that guide clinical practice guidelines and nursing care quality.
Research Evidence
The first pillar involves identifying and leveraging quality research to answer clinical questions. Nursing evidence comes from various sources. Randomized controlled trials and systematic reviews are considered the strongest, but nurses must also critically appraise qualitative research, cohort studies and expert opinions.
The process starts with formulating a clear clinical question using the PICO method (Patient/Population, Intervention, Comparison, Outcome). For example: “In elderly patients with diabetes (P), does structured patient education (I) compared to standard care (C) improve medication adherence (O)?”
Sometimes, the term PICOT with a T is used. The T stands for time and refers to the duration whereby the intervention is implemented and/or the outcomes are measured. It specifies how long the intervention should be applied or how long patients should be followed to observe meaningful results. When time is not a critical factor, the T is dropped.
Clinical Expertise
The second pillar recognizes that research alone can’t dictate patient care. Clinical expertise defines the proficiency and judgment nurses develop through time, experience and continued education. It’s essential for interpreting and applying evidence appropriately.
Patient Values and Preferences
The third pillar ensures that EBP adapts to individual needs rather than rigidly applying research findings. Nurses should integrate evidence with patients’ unique circumstances, cultural backgrounds, values and life goals. Even when strong research supports a particular intervention, nurses should advocate for treatment decisions that honor patient preferences and priorities. This involves transparent communication about options while supporting choices that align with what matters most to each patient.
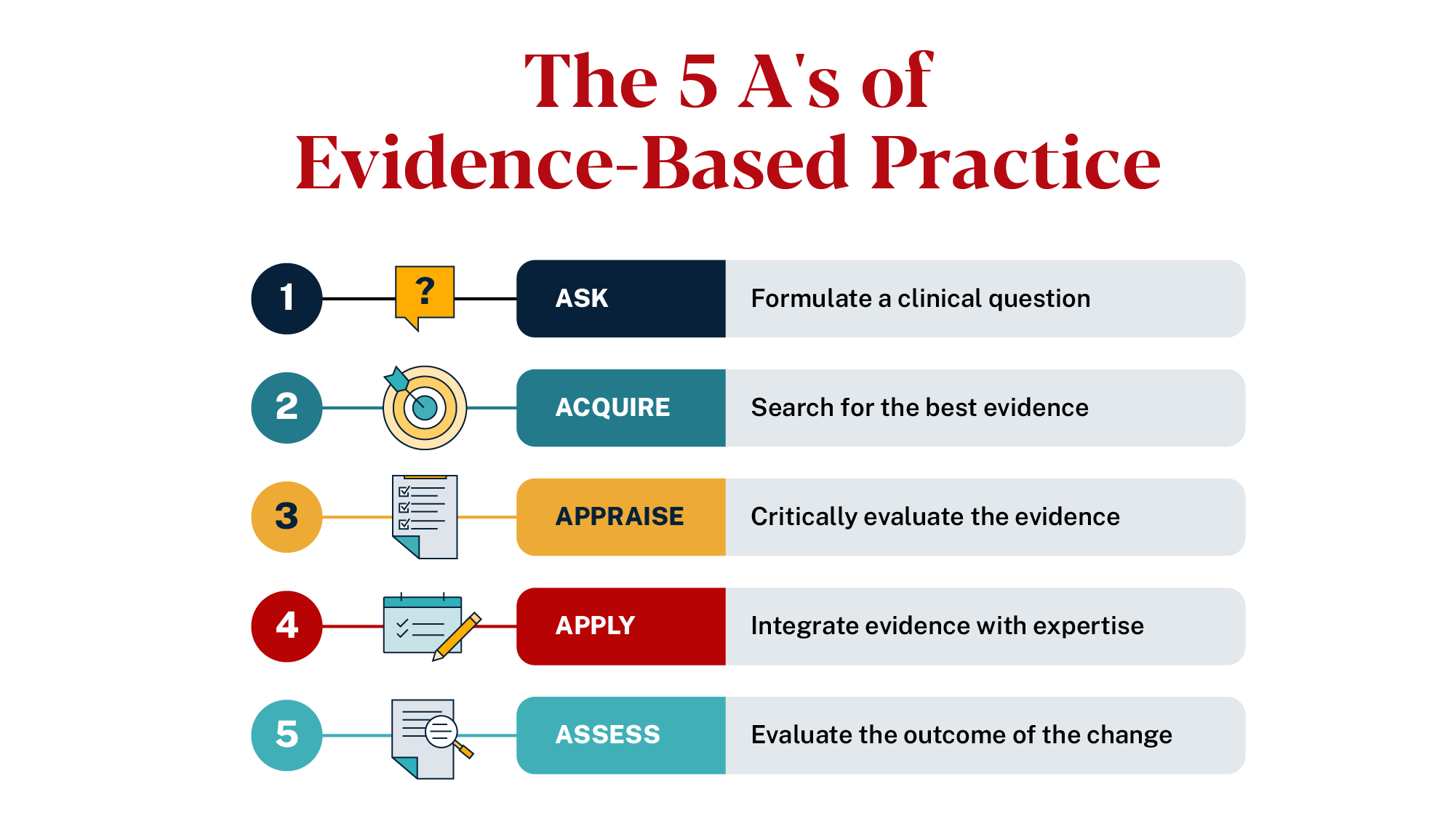
The 5 A’s: How to Implement EBP
The 5 A’s of EBP offer a structured process for integrating research into clinical decision making. By applying these steps, nurses can ensure care is evidence-based, patient-centered and contextually relevant.
- Ask: Formulate a clinical question using the PICO method
- Acquire: Search for the best evidence
- Appraise: Critically evaluate the research
- Apply: Integrate the applications with clinical expertise and patient values in mind
- Assess: Evaluate the outcomes
Evidence-Based Practice Nursing Examples
Let’s look at EBP nursing examples that can demonstrate how research transforms into practical skills and applications in common scenarios.
Example 1: Fall Prevention Protocols
Particularly in inpatient or rehabilitation settings, patients may be at varying levels of fall risk. Tools that support prevention include:
- Conducting risk assessments within 24 hours of admission, with changes of condition after a fall and quarterly
- Leveraging assistive devices like walkers, canes, shower grab bars and non-slip socks
- Monitoring and rounding regularly and encouraging patients to request assistance when needed
Example 2: Infection Control and Hand Hygiene
Medical facilities support patients’ healing but also run risk of spreading infections. Controlling infection starts with the simplest task – hand hygiene. Nurses must thoroughly wash their hands or use alcohol-based sanitizers after leaving and before entering a patient’s room, especially if the patient is immunocompromised, elderly or receiving wound care. Additional EBP tools include:
- Wearing personal protective equipment (PPE) to protect nurses and patients from infectious diseases
- Leaning on environmental services to ensure rooms are disinfected properly and regularly
- Using sterile equipment and disposing of needles and syringes appropriately
Example 3: Pain Management Best Practices
From a nursing standpoint, pain management involves administering medication and collaborating with a team of healthcare professionals, like providers and physical therapists. Examples of pain management best practices include:
- Conducting assessments, noting predispositions, onset, location, frequency, duration and other descriptive factors of pain
- Educating patients on management and safe medication use
- Monitoring patients who require opioids to ensure controlled and effective use
Example 4: Pressure Injury Prevention
A pressure injury occurs in patients who are bed-bound for extended periods of time without movement. Nurses can support prevention with measures including:
- Turning patients at regular time intervals to relieve pressure on skin and tissue
- Leveraging pressure redistribution mattresses to aid with pressure redistribution
- Conducting regular skin assessments, managing skin moisture and intervening immediately at any signs of injury
Example 5: Emergency Departments
Integrating evidence-based practices with the fast-paced nature of emergency departments can feel overwhelming, but it’s essential to ensure patients are prioritized and treated effectively. Some ways nurses can use these tools include:
- Following systematic triage protocols and assessment tools to effectively evaluate patients and the urgency or severity of their condition
- Utilizing standardized pain scales to minimize opioid use
- Involving patients in their care to ensure they understand treatment and feel safe
Barriers to Evidence-Based Practice in Nursing
Implementing EBP isn’t always easy for the nursing profession. Challenges that might come up include:
- Time limitations: Heavy workloads can disrupt nurses’ ability to engage in research and training
- Lack of access to journals: Funding restraints limit access to equipment and technology needed to implement EBP
- Training gaps: Staying current with the latest practices requires nurses to engage in continuing education
- Resistance to change: Comfort with existing methods or fear of the unknown can disrupt individual interest in EBP
- Organizational culture: Workplaces that don’t prioritize EBP or support opportunities for nurses to train can be discouraging
How Healthcare Facilities Support Evidence-Based Practice
One of the key drivers to executing EBP as a nursing standard is supportive leadership and administration. Healthcare facilities who prioritize upskilling their nurses have a greater opportunity to improve patient outcomes. They can do so with activities including:
- Workshops and EBP training
- Research librarian support
- Clinical education teams
- Standardized protocols
- Quality improvement programs
FAQs About Evidence-Based Practice in Nursing
What is the goal of EBP in nursing?
At the heart of EBP is improving patient care through the integration of clinical expertise, patient values and research. Implementing proven nursing practices strengthens nurse skillsets and improves patient outcomes.
Is EBP required in all nursing roles?
EBP isn’t required in all nursing roles, but it’s increasingly recognized as a standard of practice. It may not be formally included on a job description, but many healthcare organizations and facilities advocate for it.
What’s the difference between EBP and nursing research?
EBP focuses on implementing proven nursing practices to improve patient care, while nursing research builds scientific knowledge and understanding in the field.
Where can nurses find reliable evidence?
Databases like the Cumulative Index of Nursing and Allied Health (CINAHL), PubMed, Cochrane Library and resources from professional organizations such as the American Nurses Association and the Joanna Briggs Institute are great places to search.
Developing strong EBP skills is fundamental to professional success and providing the highest quality care that patients deserve. American College of Education (ACE) offers affordable, fully online nursing programs where you can complete your courses virtually and your practicum locally.