The field of public health is continuing to expand now more than ever. The United States Bureau of Labor Statistics reported that employment in public health is projected to increase from 2023 to 2033 across a variety of jobs: community health workers (projected to increase 13%), epidemiologists (projected to increase 19%) and health education specialists (projected to increase 7%).
These are just a few of the branches within the arena of public health careers, which includes but is not limited to epidemiology, community health, global health, public policy, maternal and child health, health equity, environmental health and biostatistics. A public health professional can stick to one specialty for years or dabble in many different areas as they progress forward in their career. This opens up boundless opportunities and room for an evolution of interests that all contribute to public health initiatives.
How I Started in Public Health
My public health career began in epidemiology at the start of the COVID-19 global pandemic. I performed contact tracing and notifying, interviewing and tracking individuals who had been exposed to an infectious agent. This opened my eyes to the critical component of data management and information privacy within the U.S. public health system.
I learned the challenges and rewards of contact tracing by conducting over a thousand interviews. I would say that 90% of the people I spoke with were more than willing to provide necessary details about their COVID-19-related predicament. Contrary to my early assumption that I would have difficulty collecting data from strangers during a time of health crisis, I found that most people were open to participate in contact tracing, which is designed to protect them and the people around them. This held true in more than one region of the U.S. where I worked.
Fast forward to recently, I served as a public health specialist where I maintained similar duties to that of a communicable disease epidemiologist. I focused on data analysis, data visualization and epidemiological reports for many different infectious diseases. It was great to see my previous experience apply to my new one. My time was spent using data software to test for significant correlations between patient attributes or exposures along with morbidity and mortality rates. This position reiterated the fact that a scientist can only perform analyses to the quality level of the data that is available.
Now, I’m able to apply my experience to pay it forward and give to the future of public health professionals by teaching nutrition science and wellness at the college level.
Why Epidemiology?
Epidemiology is the analysis and study of patterns, determinants and distribution of disease throughout a population. Methods for disease prevention and risk factors of acquiring an infection are identified by epidemiologists.
The COVID-19 impact on the U.S. led to members of different healthcare sectors, like public health and clinical medicine, learning how to trace and combat the epidemiology of an infectious disease. A communicable disease epidemiology department focuses on slowing the spread of infection through research and development initiatives. This can occur with contact tracing, case investigations, immunizations, data analyses, public service announcements, offering online and in-person educational resources and initiating community outreach programs.
How Epidemiology Outcomes Are Accomplished
Community health outcomes are improved through the power of epidemiology with intentional, long-term healthcare data reporting. Population-level health reports depend on collecting and managing a full story for each patient, which requires excellent interviews and advanced information technology. The stress of public health emergencies is lessened when community members are kept up to date on the prevalence of current health issues through strong dissemination plans and public health education processes. State and local departments of health can offer communication pertaining to medical research and updates on digital health systems, health education, facilities and services.
Public health work can be compartmentalized by local governments, nonprofits and private companies. There are certainly higher levels like state and national governments, but let’s focus on what is typical in the more abundant local governments, which is where most public health professionals work early on in their public health career. (For example, there is one New York State Department of Health, but there are 58 local health departments in New York.)
Local health departments are run within local governments and offer services like responding to public health emergencies, assessing community health needs, disseminating information and providing immunizations. Nonprofit organizations can partner with local health departments to offer services that can improve research, provide free clinics to underserved populations and raise awareness about health issues to advocate for policy changes.
Additionally, private companies offer healthcare services that are located within hospitals and other facilities where medical care is provided. They are tasked with developing pharmaceuticals and other products related to health. There is great collaboration among private companies and the public and nonprofit sectors regarding research and health initiatives.
Public Health Contractual Work
One thing I’ve learned about working in public health is that many positions are temporary and grant funded, much like freelance work. This is important because although some employers might allude to renewing your contract at the end of the assignment, it’s unfortunately not guaranteed. Grant-funded fellowships are plentiful in public health, and it can be challenging to secure long-term work if you are only applying to these positions. As with any job, you want to ensure that your desired contract offers benefits like health insurance and a retirement plan. Read the terms of employment carefully before signing on to fulfill a grant-funded contract to ensure that this is the right position for your current circumstance. In other words, do not commit to paying a new mortgage after signing a one-year grant-funded contract with an employer who is “really hoping to keep you” but lacks legitimate documentation and resources.
The wait between public health work contracts could vary for reasons beyond your control. COVID-19 produced a boost in available public health jobs because the U.S. was facing a widespread outbreak, but that boost has since receded. One of the challenges in public health is that we’re never sure exactly when something as demanding as a pandemic will occur. There’s an unpredictable factor in public health, which is incredibly exciting to some, but could cause anxiety for others. Temporary contracts can be great for people who are just starting out in the field, receive health insurance elsewhere and can afford to take breaks between employment.
How Different Public Health Teams Collaborate
It’s not uncommon to find that the different specialties of public health work interdependently, as all are valuable and contribute to form the public health system in the U.S. Whether you work in epidemiology or another branch of public health, you’ll always cross paths with other specialties. I’ll share an example.
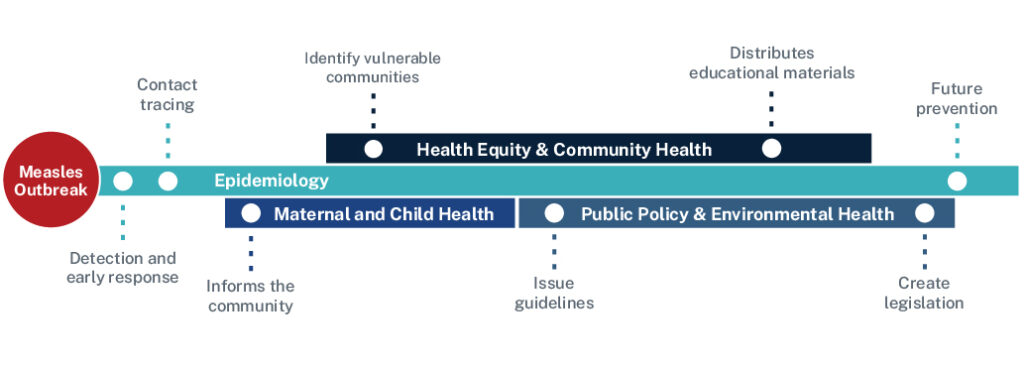
Measles is a vaccine-preventable, highly contagious and sometimes fatal airborne disease that affects people of all ages. The first measles vaccine is typically administered in childhood between 12 months and 12 years of age. A measles outbreak would be primarily covered by an epidemiology department but there are several others that could have the opportunity to contribute.
Maternal and child health teams might use educational resources provided by the epidemiology office to ensure that mothers have the information they need to protect themselves and their children. Global health offices can collaborate with biostatistics teams to better understand the global prevalence of measles and how to prepare for changes in a domestic outbreak. Health equity and community health offices can address local determinants of health that might be affecting access to immunizations and medical care. And finally, public policy and environmental health offices can create new legislation to protect the population. Public health is a network of specialized professionals who work within their departments until an outbreak strikes. Then, it’s all hands on deck to reach the goal of community health and wellness.
As you can see, working in public health services is broad and detailed at the same time. Even better, you can contribute to healthcare even if you don’t want to work on the clinical side. If this is a field you’re interested in, go for it! You’ll enjoy a rewarding career that positively impacts communities both locally and nationally.
Become the public health professional you aspire to be with the Master of Public Health program at American College of Education.